Dear all
Here is a brief case presentation of an interesting patient I saw in clinic recently. Some good clinical messages for clinical reasoning non-responsive tendinopathy patients.
If you are interested in more detailed clinical reasoning, assessment and management of tendinopathy patients please check out upcoming courses in Melbourne, Albury and Sydney.
I hope you enjoy
All the best
Peter
Key subjective information
- 33-year old female
- 1-year history of bilateral quadriceps tendinopathy
- 16 month old child
- Recently returned to office 2 days per week after second baby
Current history
- Pain onset on the right side in July 2012 and left side a few months later
- Playing netball and running regularly at time of onset and cycling road bike 80km per week
- Had been steadily increasing her running volume at time of pain onset
Load profile
- Stopped netball and running after pain onset
- Cycles occasionally 40mins and is sore for 1-2 days post
- Kneels/squats repetitively daily with young child
- Sustained deep knee flexion gardening weekends
- Walking 1-2 hrs per day, reports walking quickly
Pain profile
- Site = localized to quadriceps tendon insertion
- Aggravating factors = prolonged kneeling, gardening, cycling – can be worse for 1-2 days
- Aggravating factor = sit to stand – pain during
- Night = occasionally wakes, sleeps on side with knee flexion
- Numerical rating scale = 3/10 on average last 7 days
Relevant psychosocial factors
- Multiple failed interventions with clinicians that she feels ‘gave up on her’
- Feels she will never get better and concerned that pain is equal to damage
Patient specific functional scale
Total = 2.7/10
- Cycling 3/10
- Squatting 5/10
- Running 0/10
Past treatment
- Seen by 3 physios at highly regarded clinics. Given clams, theraband hip abduction, clinical Pilates, foam rolling, stretching hip flexors, wall squats, split squats. Also lots of manual therapy, dry needling, massage with no long term benefit
- Steroid injections x2 each side, felt better for a few weeks
Past injury profile
- Running related lateral R knee pain – diagnosed as PFJ
General health
- Nil systemic eg HTN, hyperlipidaemia, diabetes
- Normal BMI
- Regular menstrual cycle
- No significant change in symptoms with pregnancy that she could recall
- Takes the contraceptive pill, no other medications
Imaging
- MRI – bilateral quadriceps ‘tendinopathy’, chondromalacia R PFJ
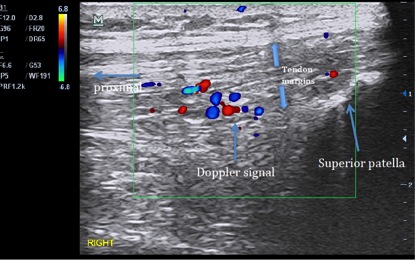
- US – see image below that I took on initial assessment, shows Doppler signal, quadriceps tendon thickening, hypoechoic change (left side was identical)
Key objective deficits
Function
1) Single leg squat
- Reproduces her pain at 60° 4-5/10
- Struggles to get beyond 60° – stiff ankle?
- Facial grimace
- Poor control hip coronal/transverse plane – not predictable pattern
- Lacks any foot pronation during squat
2) Walking
- >30° degree hip flexion IC = overstride
- <20° knee flexion in mid stance
3) Running – not assessed yet
Relevant kinetic chain assessment
- Knee to wall 8cm each side – articular restriction
- High arch with stiff passive movement midfoot, subtalar joint
- Leg extension 10RM <15kg, no pain, just ‘awarerness’
- Poor hip movement control in repeated sidelying straight leg raise
- Active knee extension -30°
- Hamstring resisted static contraction (RSC) weak in running/walking initial contact (IC) position – ie hip flexion 30°, knee flexion 10°
Knee assessment
- Full range of motion
- Tenderness on palpation quadriceps insertion into proximal patella
- No diffuse/secondary hyperalgesia
- No signs (clinical/imaging) history suggestive of common differentials including suprapatellar plicae, distal ITB, PFJ
Summary of key clinical reasoning
- Diagnosis = bilateral quadriceps tendinopathy – this diagnosis is primarily based on pain that is worse with abusive tendon load (ie compressive and energy storage load (see below) and is localized to the tendon)
- Initial related to energy storage overload in running and netball – likely overstride is carried over to running and a significant factor
- Now maintained by sustained compressive postures – squatting, kneeling with children, gardening
- Systemic drivers = nil, the fact that pregnancy had no effect indicates estrogen is not a factor
- Beliefs, thoughts = negative outlook, counterproductive beliefs about pain, very typical for someone with a long history and poor education
Significant kinetic chain and movement factors
- Movement deficits = classic case of knee is the meat in the sandwich – overloaded due to stiff ankle DF/foot and ineffective hip function in squatting
- Having said this, hip strength and control has been the focus of three prior physiotherapy interventions, strongly suggests this is not a key factor
- Quadriceps weakness/inhibition likely contributes to stiff knee squat strategy
- Hamstring restriction/end range weakness may be significant at initial contact and contribute to overstride and knee overload
Treatment plan
- Education – importantly pain beliefs and realistic goal setting
- Retrain out of knee flexion at night or use facilitators eg tape, brace
- Load manage – minimize deep knee flexion compressive postures, continue no running for time being, reduced step length and reduce walking speed
Criteria for energy storage = minimal or no pain with load tests eg hop, SL squat and adequate/improved leg extension strength
- Ankle range – calf raises into end range for length-tension benefits, ankle mobilization
- Quadriceps loading – leg extension isometric until pain with isotonic is minimal, then progress to isotonic load
- Hamstring loading into end range
Summary points and outcome to date
I have seen this patient on three occasions over 6 weeks and following appropriate load management of deep knee flexion her symptoms have settled, for the first time in a year (ie NRS 0/10, no night pain). She is now able to ride 40mins with no pain the following day. It was definitely a case of compressive activities maintaining her pain, which was initially bought on by energy storage load. Her PSFS has significantly improved from 2.7 to 5/10. Still a 0/10 for running as she is not strong enough yet for energy storage – once this is achieved she will progress through energy storage rehab and run retraining (e.g. correct cadence, overstride) and return to running. She is feeling positive that she has control over her symptoms for the first time.
What had been missing in her management?
1) addressing sleep posture
2) adequate load management of compressive quadriceps load
3) there had been a focus on coronal/transverse plane hip control when this is primarily a sagittal plane issue
4) No heavy load quadriceps loading – I got her to buy a bench press with leg extension on it and put it in her living room! They cost $200 and this works well for compliance
5) repeated steroid injections – never a good idea